NHSBT Colindale: Inside blood and transplant centre
The NHS is urging more people to donate “liquid gold”, as Britain ramps up production of plasma for life-saving medicines. Plasma is the liquid component that makes up 55% of blood and carries red cells, white cells, platelets and key proteins around the body. Antibodies found in plasma can be made into medicines for people with rare diseases who cannot produce enough of their own.
Use of UK donor plasma to make medicines was banned in 1998 as a precautionary measure against Variant Creutzfeldt–Jakob Disease (vCJD), linked to mad cow disease. The disease was spread primarily through eating beef contaminated with prions — abnormal proteins — from cattle with Bovine Spongiform Encephalopathy. It was also transmitted through blood infusions, with five such cases identified in the UK. For more than two decades, the NHS relied on overseas imports of products including immunoglobulins, which can strengthen the immune systems of people with rare diseases.

The Express went behind the scenes at NHSBT’s Colindale facility (Image: Adam Gerrard / Daily Express)
The ban was finally lifted five years ago and patients began receiving medicines made from UK plasma again in March 2025.
As the health service scales up domestic supplies, the Express visited a processing centre in London where staff work night and day to separate whole blood donations into components.
Jan Majkowski, plasma performance and efficiency lead at NHS Blood and Transplant’s (NHSBT) Colindale site, said spare plasma previously had to be incinerated.
He explained: “In the past, we could produce red cells and platelets but we couldn’t use the plasma for medicines — that was heartbreaking. Now, we don’t have to incinerate them and everything is being used, all those parts of whole blood.”
Donated plasma is used in two ways — directly in hospitals, for example to stop bleeding from trauma or surgery, or to manufacture medicines such as immunoglobulins.
Currently, around 93% of plasma collected by the NHS is filtered from whole blood donations. The remaining 7% comes from direct plasma donations, which NHSBT hopes to increase in the coming years by opening new donor centres.
Alastair Hunter, NHSBT’s head of plasma supply operations in plasma for medicines, said: “Plasma is liquid gold. It’s as vital to patient healthcare in the UK as treatments from other elements of blood donation.”
At Colindale, whole blood donations are processed on a vast manufacturing floor where staff follow meticulous steps to separate the precious components. Red cells are used to treat anaemia and blood loss, platelets can stop bleeding, and white cells can be given to patients suffering from deadly infections.
Around 1,560 pints of freshly donated blood were due to arrive on the day we visited. A whiteboard showed production targets for each component.
At one station, we watched as blood packs — already filtered to remove white cells — were loaded into a centrifuge and spun at 3,879 revolutions per minute. The speed separates the red blood cells from the plasma without damaging them.

Golden plasma sits above red cells after being spun in a centrifuge (Image: Adam Gerrard / Daily Express)
When the bags emerged, a layer of golden plasma sat on top of the red cells. A machine then pressed each pack to force the plasma into a separate bag.
Plasma must be frozen at -20C within 72 hours of donation and can be stored for up to three years. However, red cells can only be kept for 35 days at 4C, which is why the NHS needs a regular stream of donors throughout the year.
Once the bags of plasma have passed through all the necessary stations, they are stored in a -40C freezer room (the colder temperature is more energy efficient).
The plasma for medicines is then packed into boxes on pallets. Freezer lorries transport them to a cold storage facility in Reading, before they are collected by Swiss healthcare firm Octapharma, the NHS’s chosen fractionator.
Further stages are completed in Austria, Germany and Sweden, including fractionation — separating the plasma into components and turning them into medicines. The finished products are then shipped back to the UK for use by NHS patients.
These medicines are a lifeline for people like Kes Buckley, 60, who was diagnosed with a rare form of blood cancer called myelo dysplastic syndrome in her 30s.
After a stem cell transplant she developed graft versus host disease, which occurs when transplanted cells attack the recipient’s tissues. Kes takes steroids and immunosuppressive drugs which leave her prone to infection.
The Church of England priest, of Charlton, has monthly intravenous immunoglobulin infections to boost her immune system and stave off serious infections. She was one of the first patients to begin receiving immunoglobulin made from UK donors in March.
She said: “I cannot express enough gratitude to all those who donate blood or plasma. My life has been saved over and over again by the generous nature of altruistic strangers.”

Blood packs are spun at 3,879 revolutions per minute to separate components (Image: Adam Gerrard / Daily Express)
Kes added that donors had given her “precious time” to see her daughter grow up, and to welcome four grandchildren. She said: “I wish I could bottle all that generosity and kindness and share it with the world.”
The manufacturing of plasma for medicines is a complex process with countless checks to ensure quality and safety. All of this is necessary to reduce the UK’s reliance on imported supplies, which largely came from the US.
Estimates suggest that increasing the domestic supply could save the NHS £5-10 million per year. The health service began scaling up the plasma supply chain during the pandemic, when convalescent plasma collected from people who had recovered from Covid was trialled as a treatment.
Importing plasma also became more difficult during the outbreak due to border restrictions. Mr Majkowski said: “We started speaking with partners in Europe and thinking we also need to have our own plasma production.”
The ban was lifted in 2021 after rigorous scientific reviews showed no confirmed cases of vCJD transmission through plasma-derived medicines.
More than 2,200 patients have since been treated with plasma medicines made from UK donations. The NHS is now 80% self-sufficient in production of albumin — used to treat severe burns, major injury, infections, or liver disease — and 25% self-sufficient in intravenous immunoglobulin.
Mr Hunter said it was “brilliant” to see the NHS using home-grown supplies again but the health service wants to go further.
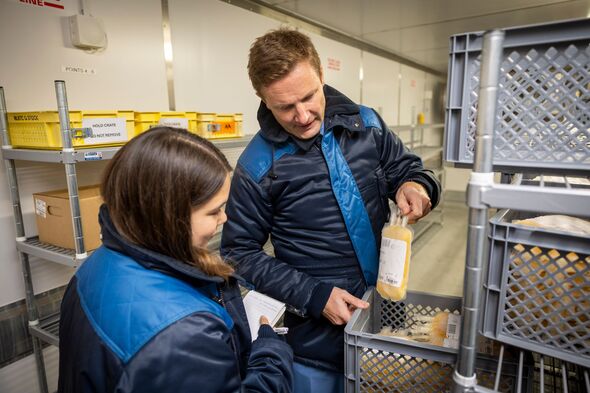
Jan Majkowski – Plasma Performance and Efficiency Lead with Hanna inside the minus 40 freezer where (Image: Adam Gerrard / Daily Express)
He added: “NHS England’s intent is to increase that percentage of self-sufficiency over the years to give us more domestic resilience.
“The benefits for patients are that plasma medicines are scarce. There are patients who may be prescribed treatment every four weeks, but because of scarcity they may have been treated every six weeks or longer.
“The additional supply allows consideration of whether we can get those treatment windows more into alignment with what is best for the patient.”
NHSBT has three donor centres in Birmingham, Reading and Twickenham where plasma alone can be filtered from donors’ blood.
Mr Hunter said: “We’re pretty much where we are with plasma recovered from whole blood…so our expansion will come from opening up new source donor centres.
“Our organisation is about saving and improving lives. The work that we’ve been doing over the last five years directly delivers that. It’s amazing to see what we’ve achieved — six months in, our plasma has treated 2,200 patients. It’s fantastic.”
He added: “We want people to keep donating whole blood, that’s the bedrock, but also to come in and donate plasma specifically. Please donate plasma.”

The frozen plasma is loaded onto a freezer lorry and taken to Reading (Image: Adam Gerrard / Daily Express)
What’s the difference between blood and plasma donation?
When you donate whole blood, around a pint of blood is collected in five to 10 minutes. This contains plasma as well as other components including red and white cells and platelets.
Plasma-specific donation takes around 30-45 minutes and involves a machine that filters your blood while you donate, so only plasma is collected. The other components are returned to your body.
Jan Majkowski, plasma performance and efficiency lead at NHS Blood and Transplant Colindale, said: “What we’re doing effectively in plasma collection is connecting a mini-centrifuge to that person which takes the whole blood, spins it, and returns the other fractions to the vein.”
Plasma donation has a shorter recovery time, so people are allowed to donate plasma as often as every two weeks.
Men can donate blood every three months and women every four months, because men typically have higher iron levels.
You can find out more about blood or plasma donation here.

Samantha receives IVIG to boost her immune system once a month (Image: NHSBT)
‘Selfless donors have changed my life’
Samantha Bloomfield remembers being plagued by colds, chest and urinary infections from a young age, often requiring treatment with antibiotics.
The 55-year-old was eventually diagnosed with Common Variable Immunodeficiency at St James’s University Hospital in Leeds in 2011.
She said: “The consultant said to me that I don’t have a sufficient immune system to be able to fight any infections. In fact, he was surprised I didn’t have every other bug going around because my levels of antibodies were so low.”
Samantha, who works as an electrical wholesaler, began receiving monthly immunoglobulin infusions (IVIG).
Each infusion takes around two hours while she sits and enjoys a cup of tea and “a biscuit, if I’m lucky”. Samantha said: “From then on, I don’t think I have had any chest infections whatsoever.
“I had to receive a few immunoglobulin infusions to build up my immunity and now, because I still don’t produce antibodies and they don’t last, I return for my top-ups so I can fight off colds like everyone else.
“Those two little hours every four weeks are life-changing for me. It really is amazing.”
Samantha, who now receives iVIG made from UK donors, added: “Please become a plasma or blood donor if you can. You will be changing the lives of so many people through your selfless donation.
“Donors are taking the time out to do their little bit, and it is very, very much appreciated. Thank you to everyone who donates.”